Ever considered living your best liver fitness summer yet? Dive in. Transform. Shine on! There’s no better season to kick-start a liver positive lifestyle! Summer, with its delicious ripe produce and array of outdoor activities, provides a perfect backdrop to consider and revamp how your daily routines can create the space to practice and promote liver wellness. With chronic hepatitis, fatty liver disease (NAFLD), and cirrhosis on the rise, particularly in at-risk communities, it’s time to change our relationship to liver health awareness. Earlier this month, the CDC reported that the mortality rate for liver cancer has gone up by 43% over the past 15 years – and that’s despite the recent development of new treatments for hepatitis C and the availability of vaccines for hepatitis A and B! So now, more than ever, we all need to incorporate a healthy dose of liver lovin’ into our daily lifestyles.
Over the past three years on World Hepatitis Day – to enlighten and rally new voices – the Al D. Rodriguez Liver Foundation, mindful of these alarming stats, has proudly rolled out three notable Liver Awareness social media events: “Top 10 Reasons to Screen, Vaccinate, Educate — Don’t Hesitate!” in 2015; “Top 10 #Hepatitis Facts on Latinos/Hispanics/Latins in the Americas” in 2016; and “Top 10 Facts for Hepatitis-Aware Tattoo Safety” in 2017.
To commemorate World Hepatitis Day 2018 and memorialize our beloved, talented friend and colleague, Al D. Rodriguez, whose life was dramatically cut short six weeks following an unexpected liver cancer diagnosis — due to chronic hepatitis – ADRLF cordially invites you to follow us, hourly on Monday, July 30th, across an inspiring, informative day as we share “10 Terrific Ways to Love Your Liver.” Our social media event highlights our Top 10 favorite tips of the season, for you to enjoy a nourishing, active, healthful summer of self-awareness and self-care with new incentives to debut your foxy new liver-healthy self!
These ‘10 Tips’ are of course in addition to ever-reliable strategies to drink moderately, monitor risky practices, be aware of symptoms – and of course, follow ADRLF’s golden advice to: SCREEN. VACCINATE. DON’T HESITATE!
In Al D.’s honor, on this day – the 10th Anniversary of his passing – we ask you to help spread the word about the risks of hepatitis and the importance of liver wellness, so that we can all: Do Better! Or better yet, Do Best!
So, check out these carefully curated tips – and let us know which ones work best for you!
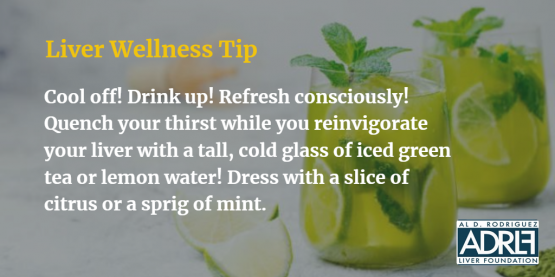
Tip #1: The summer heat calls for refreshing drinks that need not be restricted to sugary lemonades and sodas, or ice-cold beer. Green tea is a superfood beverage that contains antioxidants called catechins, which help protect the liver from toxins and free radicals that cause cellular damage and inflammation (source: http://bit.ly/2O80KBk). Infinitely more interesting than plain water, and containing numerous health benefits, those looking to cleanse their livers and/or living with chronic liver illness have “every reason to make lemon water their go to hydrating medium” (source: http://bit.ly/2JYIMy1). In fact, a recent study highlighted the hepatoprotective power of juiced lemons, especially for people with liver diseases (source: http://bit.ly/2Oa4JNX).
Blending in fruits, veggies, and ingredients filled with anti-inflammatory agents is also a great idea to create satisfyingly hearty, nutrient-rich beverages that also help the liver flush out toxins. Check out these tasty, liver-healthy smoothie ideas to beat the summer heat.
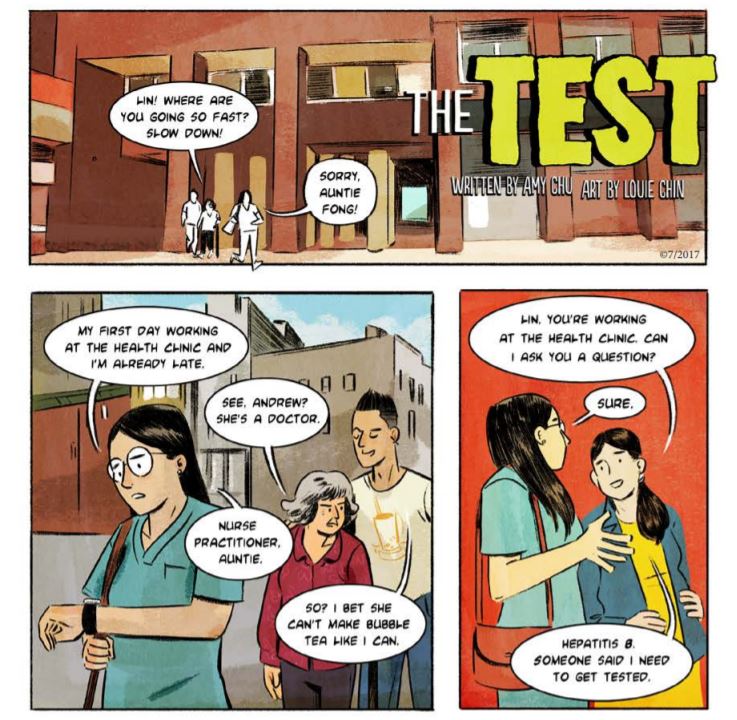
Tip #2: Hepatitis is a highly contagious disease. Hepatitis A, for example, is a common cause of foodborne infection, which led to serious outbreaks in San Diego, Nashville, and most recently in Ohio. It’s important to make a doctor’s visit to specifically check if your hepatitis A and B vaccinations are up-to-date. And if not, you know what to do!
Know the required timeline for hepatitis A vaccination here.
Find out if you need to get a vaccine for hepatitis A and B here.
Tip #3: Charcoal-grilled meats contain more carcinogens called polycyclic aromatic hydrocarbons (PAHs) than meat heated with propane. When fat drips from meat, the fat burns and creates PAH-infused smoke, which coats what you’re cooking. And charcoal makes more smoke than gas does. Also, charcoal flames are hotter, which chars meat and creates heterocyclic amines (HCAs), another carcinogen. Propane still produces some PAHs and HCAs, though, so take these steps with any grill – Trim fat! Lean meats create less drippings and less smoke, which reduces PAHs. Marinate! Soaking meat in vinegar or lemon juice reduces HCAs by 90 percent. Flip frequently! Studies have shown that turning meat frequently results in fewer HCAs (source: http://bit.ly/2Oc32Q4). We also suggest adding liver-friendly omega 3 rich fatty fish and flavorful vegetables to your cook out. Hey, a savory sizzling summer kabob is a difficult offer to resist! (source: http://bit.ly/2LWd46d)
Tip #4: A study found that prolonged sitting – that is, sitting for 10 or more hours a day – increases one’s risk of getting nonalcoholic fatty liver disease (NAFLD) by 9%. Fatty tissues can build up in the liver because of long, sedentary practices. While no medication has been approved to treat NAFLD, the best solution is to cut down on sitting time and stay physically active through lively motions like dancing and exercise. Outside of the office or even at your desk, you can also try certain yoga poses that stimulate the liver and other vital organs to function properly.
Check out this interesting movement study here.
Try these revitalizing liver-friendly yoga poses!
Tip #5: Keep the stress at bay with a relaxing massage! Massage therapies offer an oasis for tensed muscles – and for a tensed liver as well. Different kneading and rubbing movements boost the body’s overall blood circulation and reduce the accumulation of fluids in the body’s extremities that tends to cause fatigue and body aches. Enhancing blood flow through a massage promotes better liver function, as well as stimulates the processing of metabolic waste. So whether you seek out a professional and take in a spa visit, or need to mind your budget and craft your own therapeutic self-messaging routine, do know that you’re attending to your mind, body, and soul!
For liver-friendly self-massaging techniques, click here.

tip #6: Relishing the summer means heading to the beach, park, or other outdoor escapes to enjoy alfresco dining. Get creative in preparing your picnic basket and go for tasty, liver-healthy alternatives to replace traditional picnic food and beverages, like hamburgers, hotdogs, fried chicken and chips. Consider colorful, in-season fruits and vegetables, and home-made treats rather than ready-to-eat supermarket options and salty snacks. Your salad combo choices are endless! For example, carrots, beetroots, and other fruits and vegetables with red-orange pigments contain carotenoid – an antioxidant that promotes natural liver detox. Goji, blueberries, and raspberries are liver superfoods that add flavor to salads.
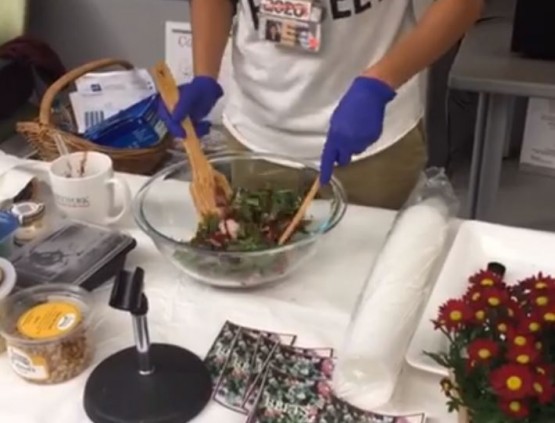
As a part of ADRLF’s commitment to promote liver health awareness, we’ve often partnered with the William F. Ryan Community Health Network to produce, inspiring, fun-filled “Love Your Liver” wellness events in New York City – including this cooking demo of a flavorful, easy-to-make, liver-friendly beet and arugula salad: http://bit.ly/2LZdKYL

Tip #7: Essential oils are highly-concentrated plant essences that have natural antiseptic properties. Chamomile, for example, helps the liver reject and discharge poisons, while fennel, geranium, and rosemary oils have anti-infectious properties and have been found to support digestive functions, balancing hormones, which contribute to overall liver health (sources: http://bit.ly/2Oea8mW, http://bit.ly/2Oea8Ds).
Tip #8: Dark chocolates contain flavonoids, which are unique antioxidants that help cleanse the liver and control blood pressure. These nutrients are especially advantageous for people with liver cirrhosis, a serious condition wherein the liver cells are replaced by tough scar tissues that impair proper liver functions. These liver scars also make it difficult for the blood to flow through the liver, resulting in the build-up of blood that may lead to a stroke and/or heart attack. The high level of antioxidants in dark chocolate helps reduce the damage in blood vessels, as well as liver scars.
Discover how dark chocolate nourishes the liver here.
Tip #9: Saunas offer relaxing ways to help the body release toxins through sweat, while getting rid of dead skin cells, improving the overall clarity of the skin, relaxing tense muscles, relieving sore body parts — and simultaneously boosting the body’s immunity. It’s known to be a great way to support liver function by flushing out toxins and revitalizing the liver through natural cleansing. However, caution is always recommended before getting into this profound sweating experience. People with conditions like hypertension or heart problems, as well as pregnant women, should consult a physician before doing sauna time. It’s also important to be well hydrated before getting inside a sauna; and to cool down after a heated session.
For more sauna benefits and precautions, click here.
Tip #10: We’re often told to stop eating a couple of hours before bedtime – but what happens when you get hungry just before powering down for the night? Sleeping with a hungry, depleted stomach (and liver) forces the brain to go into starvation mode and activates adrenal stress hormones that result in poor sleep.
Raw honey, however, has been found to contain an ideal fructose to glucose ratio to support the liver, even hours after your last meal and during your sleep or ‘night fast’ (source: http://bit.ly/2LRexhH). So, eating honey before bed ensures the body an adequate source of readily-available energy — and activates the sleep hormone, melatonin.
This is especially helpful for people with liver diseases. Sleep disturbances, such as insomnia, hypersomnia, and sleep apnea are common among people with liver disease — as they disrupt sleep patterns, while contributing to poor health and fatigue. Many people with obstructive sleep apnea are obese, which puts them at a greater risk for a fatty liver outcome. A 2012 study also found that one of the complications of liver cirrhosis is the disturbed sleep pattern. Yes, we’re all sleep-deprived, but you can turn your vital organ health around. Liver fitness needs sleep, so give the gift of proper rest to your body as regularly as you can!








 Has the term ‘Ayurveda’ crossed your radar lately? If it sounds familiar, it’s probably because it is popular within the health and wellness community. Ayurveda, also popularly known as Ayurvedic medicine, is a traditional healing practice developed in India; it literally means knowledge or science (veda) of life (ayu). This ancient holistic medical system, believed to be at least 3,000 years old, uses herbal medicines, natural treatments, and dietary practices to promote health and wellness of the mind, body, and spirit. Numerous studies and articles have noted the benefits of Ayurvedic practice to human health and wellbeing, including liver health. While generally considered alternative medicine in most parts of the world, it is definitely worth checking out.
Has the term ‘Ayurveda’ crossed your radar lately? If it sounds familiar, it’s probably because it is popular within the health and wellness community. Ayurveda, also popularly known as Ayurvedic medicine, is a traditional healing practice developed in India; it literally means knowledge or science (veda) of life (ayu). This ancient holistic medical system, believed to be at least 3,000 years old, uses herbal medicines, natural treatments, and dietary practices to promote health and wellness of the mind, body, and spirit. Numerous studies and articles have noted the benefits of Ayurvedic practice to human health and wellbeing, including liver health. While generally considered alternative medicine in most parts of the world, it is definitely worth checking out.