Embattled Essential Workers. Healthcare Heroes. Infection Blooming. Lives Lost. Economies Upended. Jobs Evaporated. Racial Imbalance. Civil Unrest. Tightened Protocols. Black Lives Matters Rising. Heightened Activism. Upside-down Days. Anxious Nights. Welcome to 2020!
COVID-19’s global pandemic may have cancelled so many important goings-on in our professional, personal, and social lives—from elective surgeries, to graduations, to travel plans—however, this critical period of hunkering down at home (for those fortunate enough to have one) does not mean forgetting about liver health! Chances are, you’ve heard this repeatedly: People with serious underlying medical conditions—including hepatitis and liver disease—might be at higher risk for severe illness from COVID-19. So, what does this mean in terms of: (1) understanding one’s risk—particularly among marginalized BIPOC (Black/Indigenous/People of Color) and LGBTQ+ communities facing healthcare inequities; (2) ensuring liver fitness to help protect against the impact of hepatitis, coronavirus, and more; and (3) accessing preventive self-care amid current physical distancing restrictions?
Despite alarming corona-era statistics and uncertainties, there is promising hope to live healthier lives through the transformative power of education, advocacy, and art—largely driven by social media. So, PLEASE SHARE OUR POSTS!
Together, we can demystify myths, illuminate facts, build more inclusive structures, and emphasize key strategies around healthfulness and hepatitis awareness at this critical time. Let ADRLF inspire you to: SCREEN. VACCINATE. DON’T HESITATE!
On this special World Hepatitis Day 2020, we invite you to join us for our lively 6th annual social media event, “LIVER WELLNESS IN THE TIME OF COVID-19,” from 10 AM to 6 PM [EST]! With new posts—every hour, on the hour—you can empower yourself with evidenced-based updates about protecting your body and liver amid this pandemic. So prep your morning meal—preferably with a tasty liver-friendly, antioxidant-rich berry smoothie or green tea lemonade (tasty recipes here: http://bit.ly/29HytBg)—and stay tuned!

Doctors reported a rare case of a COVID-19 patient who developed acute hepatitis before any respiratory symptoms. Learn more: https://bit.ly/3eSCxeI
Like coronavirus, hepatitis E is spread via contamination and unsanitary practices. Learn more about hepatitis E & staying squeaky clean here: ow.ly/Ok0c50AKi7T
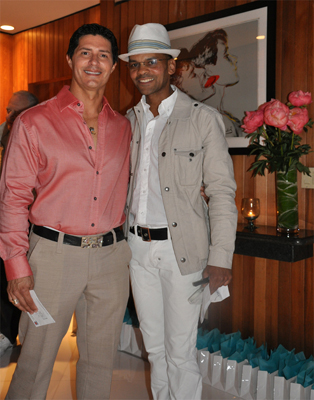
Virus screenings save lives! Our very own Al D. Rodriguez, a celebrated actor, battled briefly with liver cancer, following an asymptomatic period of chronic infection with the Hepatitis Virus. Know his story! http://ow.ly/kNcJ50AKn9a
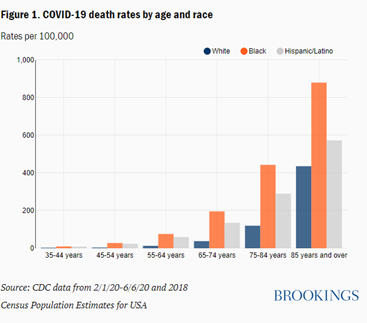
Stand up for BIPOC communities, as [COVID-19 and liver disease] death tolls rise in the Americas. Understand racial health disparities & advocate for better access to quality medical care. http://ow.ly/jCh950AKrku
From dancing, to yoga, to running with your dog—keep moving to invigorate liver function with these wellness tips: http://ow.ly/27yA50AKsAY
Stay up-to-date on potential treatments for the novel coronavirus—including this celebrated #HepC treatment shown to accelerate patient recovery! Read the latest: https://bit.ly/32PLLWK
Work in healthcare? Occupational exposure is real. Keep up with your vaccines to protect yourself, your patients & your community. http://bit.ly/2Z9ZWFf
Dispel harmful stigmas and myths that spur more disparity! Share facts and positive attitudes that promote equality and respect! https://bit.ly/2OuTfG1
Sleep health + liver health go hand in hand!Get a restful sleep amid #COVID19 and other social stress anxieties with these tips: http://ow.ly/GdsY50AKFYi
Still sheltering in place? Try telehealth to stay safely connected with your doctor for a range of illness prevention, management and treatment—of hepatitis and beyond… http://ow.ly/ejxY50AKG0N

With approximately 4.1 million coronavirus cases in the U.S, according to WHO, and over 646,000 deaths to date worldwide, the intensely brutal COVID-19 pandemic has swiftly, intimately, and destructively re-shaped the world as we know it. The Al D. Rodriguez Liver Foundation would like to take a moment of silence for the countless lives lost, bodies impaired, and families/loved ones impacted by the COVID-19 pandemic, thus far. We must look forward to harnessing solutions, while moving together through collective stress, grief, and transformation. According to the Pan American Health Organization (PAHO), “3 out of 10 people in the Americas are at increased risk for COVID-19 due to underlying health conditions.” With so many vulnerable populations living with disabilities and battling illnesses—from hepatitis, to hypertension, from diabetes to kidney disease, and beyond—ADRLF would like to extend a heartfelt THANK YOU to the legions of dedicated, overworked, and underpaid healthcare providers, first responders, and essential/safety workers tirelessly navigating their way through our health crisis to help save lives and provide medical care. As well, we share deep gratitude with the masses of equality-demanding activists and advocates dedicated to making lasting structural change. These various frontline workers continue to fight and put their lives at risk in the hopes of creating a better, safer, more equitable world, as we forge, together, through these unprecedented times—but now with amplified, re-energized voices. Keep informed, take time to care for yourself and others, practice protocols, reduce stress, embrace wellness goals—and please stay healthy! To that end, as we continue to promote hep awareness and liver wellness, ADRLF lovingly urges you to: Screen. Vaccinate. Don’t Hesitate!
To understand more about your risk of COVID-19 and liver disease, visit our blog.
To get updates of COVID-19, visit the WHO site.
For information about underlying medical conditions and COVID-19, click here.